Doula, master's of public health graduate, new IBCLC, and feminist. I'm reflecting on my studies, reflecting on other people's studies, posting news, telling stories, and inviting discussion on reproductive health from birth control to birth to bra fitting.
Tuesday, February 23, 2010
Home birth insurance reimbursement by NYS insurance
When I was in NYC, I met two Columbia journalism students who were doing a project on home birth. I didn't realize it till just now, but their project is up online. It looks like a lot of the videos aren't working, which is a bummer. The interactives are still functional, though (and the web design skills are impressive!) My favorite is this chart of reimbursement for home birth by insurance type. It may no longer be up-to-date, but what a great idea! It would be helpful to have something like this for every state.
Monday, February 22, 2010
Stages of birth thinking (yes, I need a way better name for this)
Do you ever feel that there's some kind of Kubler-Ross-esque "Stages of Learning" that people go through when learning about unmedicated/physiological/natural/etc. birth?
I have been pondering this topic for a while and was sparked by this post from Navelgazing Midwife. She talks about how when she started being involved in birth/breastfeeding, she had the true zeal of a new convert. Over time, her dogmatism waned even as she watched others experience it.
While not everyone may make their dogmatic thinking external by telling it to everyone they know, I do think that almost everyone goes through that stage for a while. And it's interesting to me to watch it in myself, in people I know in person, and in blogs. In my draft version, the stages go something like this:
1. Pre-contemplation (yes, for lack of a better word I'm snagging this term from theories of health behavior change)
We are all part of a birth culture, the question is - what culture? For people in the pre-contemplation stage, it is our mainstream birth culture. This generally means that birth education comes from mass media portrayals of pregnancy and birth, as well as personal stories from friends and family that may vary greatly, but are usually filtered through the prism of our culture's main messages about birth: Painful and pathological; done in a hospital, with doctors. You might prefer a vaginal delivery or a c-section, but there's little you can do to control the outcome, and all hospitals/doctors practice more or less the same way.
2. Initial learning & revelation: This can be done through personal interest (I'm curious about birth so I'm going to learn about it), personal necessity (I'm pregnant so I'm going to learn about it), knowing someone who talks about it, deciding to go through a doula training, academic studies, or seeing a movie like "Business of Being Born". It can also be sparked by personal event like experiencing a high-intervention labor or having an unexpected c-section, that push someone to learn more.
Learning at this point is pure and exciting, what I think of as the revelation stage: "Wow! Nobody ever told me that birth could be amazing, not scary! These home births are beautiful. I didn't realize that my/my friend's/my aunt's c-section could have been prevented. I didn't know about all these harmful complications of interventions - I've only heard good things. And it's so clear how once you start one intervention, you get a cascade of them. Doctors don't have the best outcomes - midwives do! Breastfeeding has benefits I didn't know about, and they are so important. I didn't realize that I/my sister/my friend could have breastfed just by doing things differently."
There can also be anger: "Who are these butchers cutting unnecessary episiotomies? Who would ever induce a woman without absolutely clear indications? There are clearly a bunch of money-grubbing jerks out there putting women's health at risk."
To me at that point, things seemed very clear-cut. If you did x, y, and z "right", then you should get a good outcome. Certainly, you'd be foolish to do them otherwise, as that would invite disaster (right? I mean, you MIGHT escape a c-section if you get an epidural, but why would you RISK it?) These things were all true, right? So why would they not apply to everybody, in every situation?
3. Validation (or not) through experience
Of course, all this great theory has to survive the practice. Not all experiences will conform to one simple worldview.
I think the vast majority of birth attendants see such a volume of births that ultimately, nothing can happen but that their enthusiasm is tempered. Within a few births, my preconceived notions of what "should" happen at a birth began to fall away. A year of attending births nudged me yet farther away from my starry-eyed novice doula perspective. Not all c-sections can be avoided, even if you do everything "right". Sometimes epidurals are the best tool you have. Pitocin isn't fun, but it's not the end of the world. While it might be difficult to accomplish, you actually can have a great low-intervention birth in a hospital. This tempering is slow, and less personal - it's not happening to you, and it's happening over a multitude of experiences. This can also happen if you read many kinds of birth stories, or research birth extensively.
Other people come to this place from personal experience: "I hired a midwife and a doula and took Bradley classes and did visualizations and I still had a c-section. So something here isn't right." "I thought my OB was going to be a horrible witch but actually she was amazing and was nothing but supportive, and held my hand when I was crying, while the midwife was actually kind of a jerk." Or "I thought the epidural was the devil itself, but when I got one it was actually awesome and helped me have a vaginal birth."
Someone who has births that don't challenge their views, and is able to dismiss or explain away other experiences she hears about, may be able to keep believing a very one-note version. (This is where the "What if" game comes in - "Oh, you hired a midwife and a doula and took Bradley and did visualizations but you DIDN'T do yoga? There's your problem right there. What if you had? You probably wouldn't have had that c-section.")
4. Integration
As a birth attendant, I slowly was able to adjust to a more nuanced view. I think the same goes for most people who attend many births. You recognize that every situation is individual, even though there are patterns and large-scale effects that are likely, because you have a chance to see many.
For women whose experiences contradicted their original views, it's a much more personal experience. I've noticed that some people feel betrayed or angry at people, books, or classes that were part of forming their original mindset, or that they now see as not presenting a balanced picture. They sometimes just reject those ideas outright - so many of them proved to be wrong that the whole worldview is now worthless. Others are able adjust their view: "I feel confident that my c-section was necessary, whereas before I might not have been able to see that. I still see that there's still a problem with high c-section rates."
There's most certainly an ongoing aspect of this. I adjust my thoughts almost every day as I learn and think about things more; it's a process, not an endpoint, and to me embodies the simple acceptance that life (including birth/breastfeeding/parenting/etc.) is complicated.
Thoughts? It's struck me recently how hard it is to have conversations with people at different stages (especially on the internets). And how hard it is to feel represented by someone who might never have had to adjust their worldview from the "birth is safe! only intervention is dangerous!" phase, or to try to discuss c-section rates with people who have never even contemplated them.
I have been pondering this topic for a while and was sparked by this post from Navelgazing Midwife. She talks about how when she started being involved in birth/breastfeeding, she had the true zeal of a new convert. Over time, her dogmatism waned even as she watched others experience it.
While not everyone may make their dogmatic thinking external by telling it to everyone they know, I do think that almost everyone goes through that stage for a while. And it's interesting to me to watch it in myself, in people I know in person, and in blogs. In my draft version, the stages go something like this:
1. Pre-contemplation (yes, for lack of a better word I'm snagging this term from theories of health behavior change)
We are all part of a birth culture, the question is - what culture? For people in the pre-contemplation stage, it is our mainstream birth culture. This generally means that birth education comes from mass media portrayals of pregnancy and birth, as well as personal stories from friends and family that may vary greatly, but are usually filtered through the prism of our culture's main messages about birth: Painful and pathological; done in a hospital, with doctors. You might prefer a vaginal delivery or a c-section, but there's little you can do to control the outcome, and all hospitals/doctors practice more or less the same way.
2. Initial learning & revelation: This can be done through personal interest (I'm curious about birth so I'm going to learn about it), personal necessity (I'm pregnant so I'm going to learn about it), knowing someone who talks about it, deciding to go through a doula training, academic studies, or seeing a movie like "Business of Being Born". It can also be sparked by personal event like experiencing a high-intervention labor or having an unexpected c-section, that push someone to learn more.
Learning at this point is pure and exciting, what I think of as the revelation stage: "Wow! Nobody ever told me that birth could be amazing, not scary! These home births are beautiful. I didn't realize that my/my friend's/my aunt's c-section could have been prevented. I didn't know about all these harmful complications of interventions - I've only heard good things. And it's so clear how once you start one intervention, you get a cascade of them. Doctors don't have the best outcomes - midwives do! Breastfeeding has benefits I didn't know about, and they are so important. I didn't realize that I/my sister/my friend could have breastfed just by doing things differently."
There can also be anger: "Who are these butchers cutting unnecessary episiotomies? Who would ever induce a woman without absolutely clear indications? There are clearly a bunch of money-grubbing jerks out there putting women's health at risk."
To me at that point, things seemed very clear-cut. If you did x, y, and z "right", then you should get a good outcome. Certainly, you'd be foolish to do them otherwise, as that would invite disaster (right? I mean, you MIGHT escape a c-section if you get an epidural, but why would you RISK it?) These things were all true, right? So why would they not apply to everybody, in every situation?
3. Validation (or not) through experience
Of course, all this great theory has to survive the practice. Not all experiences will conform to one simple worldview.
I think the vast majority of birth attendants see such a volume of births that ultimately, nothing can happen but that their enthusiasm is tempered. Within a few births, my preconceived notions of what "should" happen at a birth began to fall away. A year of attending births nudged me yet farther away from my starry-eyed novice doula perspective. Not all c-sections can be avoided, even if you do everything "right". Sometimes epidurals are the best tool you have. Pitocin isn't fun, but it's not the end of the world. While it might be difficult to accomplish, you actually can have a great low-intervention birth in a hospital. This tempering is slow, and less personal - it's not happening to you, and it's happening over a multitude of experiences. This can also happen if you read many kinds of birth stories, or research birth extensively.
Other people come to this place from personal experience: "I hired a midwife and a doula and took Bradley classes and did visualizations and I still had a c-section. So something here isn't right." "I thought my OB was going to be a horrible witch but actually she was amazing and was nothing but supportive, and held my hand when I was crying, while the midwife was actually kind of a jerk." Or "I thought the epidural was the devil itself, but when I got one it was actually awesome and helped me have a vaginal birth."
Someone who has births that don't challenge their views, and is able to dismiss or explain away other experiences she hears about, may be able to keep believing a very one-note version. (This is where the "What if" game comes in - "Oh, you hired a midwife and a doula and took Bradley and did visualizations but you DIDN'T do yoga? There's your problem right there. What if you had? You probably wouldn't have had that c-section.")
4. Integration
As a birth attendant, I slowly was able to adjust to a more nuanced view. I think the same goes for most people who attend many births. You recognize that every situation is individual, even though there are patterns and large-scale effects that are likely, because you have a chance to see many.
For women whose experiences contradicted their original views, it's a much more personal experience. I've noticed that some people feel betrayed or angry at people, books, or classes that were part of forming their original mindset, or that they now see as not presenting a balanced picture. They sometimes just reject those ideas outright - so many of them proved to be wrong that the whole worldview is now worthless. Others are able adjust their view: "I feel confident that my c-section was necessary, whereas before I might not have been able to see that. I still see that there's still a problem with high c-section rates."
There's most certainly an ongoing aspect of this. I adjust my thoughts almost every day as I learn and think about things more; it's a process, not an endpoint, and to me embodies the simple acceptance that life (including birth/breastfeeding/parenting/etc.) is complicated.
Thoughts? It's struck me recently how hard it is to have conversations with people at different stages (especially on the internets). And how hard it is to feel represented by someone who might never have had to adjust their worldview from the "birth is safe! only intervention is dangerous!" phase, or to try to discuss c-section rates with people who have never even contemplated them.
Friday, February 19, 2010
Survey on breastfeeding and childhood sexual abuse
From an e-mail I received through a listserv:
"Childhood sexual abuse is a very common experience among American women, and is known to have significant consequences throughout the lifespan. The lack of public health analysis of child sexual abuse means that we have major limitations as to how we can work to prevent this problem, and how we can help survivors when it occurs. Childhood sexual abuse can impact women’s experiences of breastfeeding, but there is very little information about how. By sharing their stories, women can teach public health professionals about what the problems and opportunities are, and how they can respond.
To this end, I have created a survey where women are able to share their experiences. By clicking HERE, you can learn more about the survey, and complete the survey. It’s pretty open-ended so that people can take as much space as they need to write about their experiences with breastfeeding, and how they may have been impacted by childhood sexual abuse. The stories will be shared, with no identifying information, at the Breastfeeding & Feminism Symposium, as well as being part of an exciting new book due out Fall 2010. Since there is a time crunch, please complete the survey by Friday, February 26."
I think this is an important and largely unexplored topic, other than observations of LCs who I've heard at trainings or who have written articles. It would be great to hear the voices of women who have experience with this.
"Childhood sexual abuse is a very common experience among American women, and is known to have significant consequences throughout the lifespan. The lack of public health analysis of child sexual abuse means that we have major limitations as to how we can work to prevent this problem, and how we can help survivors when it occurs. Childhood sexual abuse can impact women’s experiences of breastfeeding, but there is very little information about how. By sharing their stories, women can teach public health professionals about what the problems and opportunities are, and how they can respond.
To this end, I have created a survey where women are able to share their experiences. By clicking HERE, you can learn more about the survey, and complete the survey. It’s pretty open-ended so that people can take as much space as they need to write about their experiences with breastfeeding, and how they may have been impacted by childhood sexual abuse. The stories will be shared, with no identifying information, at the Breastfeeding & Feminism Symposium, as well as being part of an exciting new book due out Fall 2010. Since there is a time crunch, please complete the survey by Friday, February 26."
I think this is an important and largely unexplored topic, other than observations of LCs who I've heard at trainings or who have written articles. It would be great to hear the voices of women who have experience with this.
Thursday, February 18, 2010
Great things nurses do
Remember when I wrote a grouchy post about unhelpful nurses? And I promised to write a post about all the great things nurses do?
Well here's an example of one!
Other great things that I have personally witnessed:
- Standing and holding the fetal & contraction monitors in place, or adjusting them over and over, without ever making mom feel guilty for being in whatever position is best for her
- Taking the monitors OFF the second they're no longer mandatory!
- Offering enthusiastic help and practical support - "Do you want a hot pad? a birth ball? what can I bring you guys?" - or offering to push on mom's back or massage her shoulders
- Nudging the doctor towards trying different positions to push in
- Doing all newborn assessments while baby is on mom's chest, even though she's the only person in the hospital doing it
- Even when I can sense that they're not personally so into unmedicated birth, never saying otherwise or being anything but positive and supportive with mom
- Getting bossy when it's hard for me to be - they must teach that special brisk, no-nonsense voice in nursing school! "Let's get you out of bed and into the rocking chair, let's go!"
- Not asking constantly for pain scores when mom is working on an unmedicated labor
- Bugging the anesthesiologist to come back and re-place an ineffective epidural
- Turning the Pit down or off as soon as they see they can
- When her shift ends, staying over if it's close to the end, or recruiting someone she knows will be supportive for the next shift
- And of course, welcoming and teaming up with doulas to help birthing women!
While it's so helpful to have the care provider (doc or CNM) be on board with what mom wants, and ultimately they will call the shots, NOTHING sets the environment of the birthing room like a great nurse! And if we're lucky, she holds sway with the care provider too!
Thank you, nurses!
Well here's an example of one!
Other great things that I have personally witnessed:
- Standing and holding the fetal & contraction monitors in place, or adjusting them over and over, without ever making mom feel guilty for being in whatever position is best for her
- Taking the monitors OFF the second they're no longer mandatory!
- Offering enthusiastic help and practical support - "Do you want a hot pad? a birth ball? what can I bring you guys?" - or offering to push on mom's back or massage her shoulders
- Nudging the doctor towards trying different positions to push in
- Doing all newborn assessments while baby is on mom's chest, even though she's the only person in the hospital doing it
- Even when I can sense that they're not personally so into unmedicated birth, never saying otherwise or being anything but positive and supportive with mom
- Getting bossy when it's hard for me to be - they must teach that special brisk, no-nonsense voice in nursing school! "Let's get you out of bed and into the rocking chair, let's go!"
- Not asking constantly for pain scores when mom is working on an unmedicated labor
- Bugging the anesthesiologist to come back and re-place an ineffective epidural
- Turning the Pit down or off as soon as they see they can
- When her shift ends, staying over if it's close to the end, or recruiting someone she knows will be supportive for the next shift
- And of course, welcoming and teaming up with doulas to help birthing women!
While it's so helpful to have the care provider (doc or CNM) be on board with what mom wants, and ultimately they will call the shots, NOTHING sets the environment of the birthing room like a great nurse! And if we're lucky, she holds sway with the care provider too!
Thank you, nurses!
Saturday, February 13, 2010
Link party!
First of all, Happy Olympics! I am so excited. I love the Olympics. My department had an Olympics party last night - come as your favorite athlete, sport, or country. We had everything from Brian Boitano to bobsledding to several people all in white ("Winter") and one Olympic torch. I was Sweden, which is a good Winter Olympics country to pick.
I've been trying to come up with some kind of play on words with the Olympics starting, Olympic rings, the rings are linked, links...I think I'm trying too hard. So let's just say that my Google Reader starred list is becoming too long to contemplate, and that it's time for a link party. I've been saving some of these up thinking "I'll write a post on this!" but the truth is, I might or might not eventually, and in the meantime why let the starred list get longer?
Academic review article on the risks of not breastfeeding for mothers and infants, and the role of obstetricians and hospitals in breastfeeding promotion. A very nice summary.
Via Empowering Birth blog, an informed consent roleplay. Has anyone ever used this with a class? It seems like a great idea to get people prepared to actually advocate for themselves - it's easy to talk about it beforehand, and harder to actually do in the moment.
And another link from Enjoy Birth about choosing hospitals wisely.
A dad talks about his thoughts on breastfeeding.
At Guerilla Mama Medicine, HUGELY important questions and thoughts about race and the natural childbirth movement.
An article from RH Reality Check about The Doula Project, which provides doulas for women who are having abortions and who are relinquishing their babies for adoption. I'm proud to say that I know one of the co-founders, Lauren Mitchell, who has an awesome quote in the piece: "You can't speak for your client, even if what's going on is the opposite of what she wanted - you're not in control of the room. But you are in control of what you are giving your client, and that is an informed ally and a deeply empathetic presence. When you're a doula you have to acknowledge how to be 'human' even when you want to be more than that. What keeps me going is the feedback from the clients that the space that I've created for them is unique and extremely important." If I end up back in NYC I would LOVE to volunteer with them!
From Birth Sense, thoughts about manual rotation of the fetal head. I have seen this happen once, and it was very effective - baby went from making very little progress with pushes, to crowning within minutes. But the midwife writing the article reminds us that it's also extremely important to move the mother!
I've also been enjoying Birth Sense's series, "Your Doctor or Midwife Still Does WHAT?" Here's a sample: #5, Cervical Exams. Reading expectant mothers' blogs I come across so many sighing with frustration that they're still not dilated at all, when is this baby going to come, etc. etc. Since there are very few actual medical reasons to do a cervical exam, it starts to seem like a highly effective method of psychological priming for induction.
Navelgazing Midwife did a great series of photo posts called "Teachable Moments" about placentas, vernix, trailing membranes, etc. Here's a great one on being born in the caul. I guess I should put in a disclaimer that these photos involve vaginas and birth fluids and stuff like that, although I have such a high tolerance at this point I have to remind myself that somebody else might need a warning.
That's all for now - off to watch me some Olympics!
I've been trying to come up with some kind of play on words with the Olympics starting, Olympic rings, the rings are linked, links...I think I'm trying too hard. So let's just say that my Google Reader starred list is becoming too long to contemplate, and that it's time for a link party. I've been saving some of these up thinking "I'll write a post on this!" but the truth is, I might or might not eventually, and in the meantime why let the starred list get longer?
Academic review article on the risks of not breastfeeding for mothers and infants, and the role of obstetricians and hospitals in breastfeeding promotion. A very nice summary.
Via Empowering Birth blog, an informed consent roleplay. Has anyone ever used this with a class? It seems like a great idea to get people prepared to actually advocate for themselves - it's easy to talk about it beforehand, and harder to actually do in the moment.
And another link from Enjoy Birth about choosing hospitals wisely.
A dad talks about his thoughts on breastfeeding.
At Guerilla Mama Medicine, HUGELY important questions and thoughts about race and the natural childbirth movement.
An article from RH Reality Check about The Doula Project, which provides doulas for women who are having abortions and who are relinquishing their babies for adoption. I'm proud to say that I know one of the co-founders, Lauren Mitchell, who has an awesome quote in the piece: "You can't speak for your client, even if what's going on is the opposite of what she wanted - you're not in control of the room. But you are in control of what you are giving your client, and that is an informed ally and a deeply empathetic presence. When you're a doula you have to acknowledge how to be 'human' even when you want to be more than that. What keeps me going is the feedback from the clients that the space that I've created for them is unique and extremely important." If I end up back in NYC I would LOVE to volunteer with them!
From Birth Sense, thoughts about manual rotation of the fetal head. I have seen this happen once, and it was very effective - baby went from making very little progress with pushes, to crowning within minutes. But the midwife writing the article reminds us that it's also extremely important to move the mother!
I've also been enjoying Birth Sense's series, "Your Doctor or Midwife Still Does WHAT?" Here's a sample: #5, Cervical Exams. Reading expectant mothers' blogs I come across so many sighing with frustration that they're still not dilated at all, when is this baby going to come, etc. etc. Since there are very few actual medical reasons to do a cervical exam, it starts to seem like a highly effective method of psychological priming for induction.
Navelgazing Midwife did a great series of photo posts called "Teachable Moments" about placentas, vernix, trailing membranes, etc. Here's a great one on being born in the caul. I guess I should put in a disclaimer that these photos involve vaginas and birth fluids and stuff like that, although I have such a high tolerance at this point I have to remind myself that somebody else might need a warning.
That's all for now - off to watch me some Olympics!
Tuesday, February 9, 2010
I love this post, found through the Lamaze Healthy Birth Carnival #4 (Avoid unnecessary interventions) about interventions hidden in plain sight. I have to admit, as a doula I am sometimes surprised by how people who are ready to advocate for their intervention-free birth barely notice or easily consent to many of these. And of course, it gets to the point where it's easy to just stop noticing them. My favorites:
It may sound odd, but when I see a woman on the L&D floor checking in, still wearing her own clothes, I take a moment to enjoy seeing her still owning her own body. I want to qualify that quickly by saying that there's nothing about choosing to wear a hospital gown, especially if you'd rather not risk sacrificing any of your own clothes, that makes you suddenly surrender all of your independent thoughts and rights. But there is something about that symbolic moment of changing into the hospital gown that so often denotes the moment when the woman is no longer in control, and that codes her in the eyes of the hospital staff as "patient".
Anyway, check out the whole post, and all the others from the Carnival!
* The uniform -Asking and expecting the mother to give up her clothes for the hospital gown.
* Who’s on first? – If care provider is part of a large practice or on-call group a woman may have never met or have any knowledge of the person who’s practice style and philosophy is helping to guide and steer her labor and delivery. On-call CP may or may not adhere to the birth plan the laboring woman worked out with her own CP.
* The big drag around – Requiring IV running with absence of medical need.
* Ice chips and Jello – Disallowing snacks and sometimes even actual water even though labor is hard work.
* One is enough – Limiting the amount or type of support persons a woman is allowed to have with her.
It may sound odd, but when I see a woman on the L&D floor checking in, still wearing her own clothes, I take a moment to enjoy seeing her still owning her own body. I want to qualify that quickly by saying that there's nothing about choosing to wear a hospital gown, especially if you'd rather not risk sacrificing any of your own clothes, that makes you suddenly surrender all of your independent thoughts and rights. But there is something about that symbolic moment of changing into the hospital gown that so often denotes the moment when the woman is no longer in control, and that codes her in the eyes of the hospital staff as "patient".
Anyway, check out the whole post, and all the others from the Carnival!
Monday, February 8, 2010
"Born Too Soon"
Watching this documentary reminds me of the great posts on Reality Rounds about avoiding the realities of prematurity. Here is a documentary that does NOT avoid them, and highlights the problems not only of early premature birth but also late-term prematurity, and the health disparities in preterm birth in this country.
It's called "Born Too Soon" and is a collaboration between March of Dimes and Kentucky Educational Television. Most of the officials interviewed are from Kentucky, and there's a focus on the rising prematurity rate in Kentucky, but it's generalizable across the country and everything that's happening there is happening around the country. I also love the doula interview, and highlighting the CenteringPregnancy model of care. I think it's an accessible, good overview of the prematurity problem (although let me just insert a little "ack!" here for the baby bottle imagery used. I am of course not a fan of coding "baby" as "bottle".)
You can watch the whole documentary here.
It's called "Born Too Soon" and is a collaboration between March of Dimes and Kentucky Educational Television. Most of the officials interviewed are from Kentucky, and there's a focus on the rising prematurity rate in Kentucky, but it's generalizable across the country and everything that's happening there is happening around the country. I also love the doula interview, and highlighting the CenteringPregnancy model of care. I think it's an accessible, good overview of the prematurity problem (although let me just insert a little "ack!" here for the baby bottle imagery used. I am of course not a fan of coding "baby" as "bottle".)
You can watch the whole documentary here.
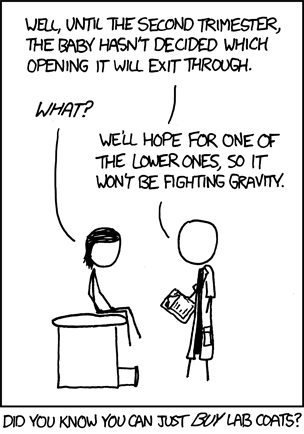
Xkcd for the maternity care win!
Friday, February 5, 2010
Friday night movie (trailer)
I've been looking at clips from a documentary currently being filmed about Maternidad La Luz. I first heard of Maternidad La Luz through a student several years ahead of me in undergrad, who did her own version of "junior year abroad" to become a midwife in Maternidad La Luz's One-Year Program. (At least as cool as partying somewhere in Europe!) After that, she returned to college and wrote her senior thesis summarizing her experience and evaluating a model for childbirth education, which I then found, read, and was amazed by.
Since then I've met several people who interned or trained at Maternidad La Luz, and wow...it sounds awesome! Watching the clips from the documentary, it looks awesome too. The homelike setting, the quiet chatter and bustle of life going on in the background, the gentle care by the midwives. I especially loved listening to their fluent "vagina Spanish" (as a nurse once termed her highly labor-focused language skills!) - it brought me back to my time in Denver, where at least half of our doula clients were Spanish-speaking only, and we did so many breastfeeding consults in Spanish that it felt strange to do one in English. I heard that familiar cadence of the phrase you've asked a hundred times - "Como le va con el dar el pecho?" "Se siente presión?" etc.
I'm looking forward to the whole documentary - I hope it will be out soon.
Thanks to my classmate and fellow LC trainee Jenna for the link!
Since then I've met several people who interned or trained at Maternidad La Luz, and wow...it sounds awesome! Watching the clips from the documentary, it looks awesome too. The homelike setting, the quiet chatter and bustle of life going on in the background, the gentle care by the midwives. I especially loved listening to their fluent "vagina Spanish" (as a nurse once termed her highly labor-focused language skills!) - it brought me back to my time in Denver, where at least half of our doula clients were Spanish-speaking only, and we did so many breastfeeding consults in Spanish that it felt strange to do one in English. I heard that familiar cadence of the phrase you've asked a hundred times - "Como le va con el dar el pecho?" "Se siente presión?" etc.
I'm looking forward to the whole documentary - I hope it will be out soon.
Thanks to my classmate and fellow LC trainee Jenna for the link!
Tuesday, February 2, 2010
Breastfeeding & medications
A frequent reason for mothers to be told to stop breastfeeding and/or "pump and dump" is because they are on medications. I hear this is particularly prevalent in emergency rooms - I assume because ER docs get so few opportunities for education, don't know their resources, and need to cover themselves for liability reasons. But many doctors, including regular primary care providers and even people who should be experienced enough with breastfeeding, like pediatricians and OBs, give bad information about breastfeeding while using medications.
This is not, of course, all their fault. As La Leche League notes, "Health care givers often turn to the Physicians' Desk Reference (the PDR) for information about drugs. ... Information in the PDR comes directly from pharmaceutical companies, whose first concern is avoiding liability. When there are no studies that prove beyond a doubt that a drug is safe for nursing mothers, the drug companies must advise against using it while breastfeeding - even if what is known about the drug suggests that there is little cause for concern."
What resources your doctor uses to determine the safety of medication can make a big difference. One study used a list of drugs that were commonly prescribed to breastfeeding mothers, and looked how many were considered safe in frequently consulted resources:

From Akus M, Bartick M. Lactation Safety Recommendations and Reliability Compared in 10 Medication Resources Ann Pharmacother. September 2007;41(9):1352-1360.
As you can see, there are much better resources out there than the PDR! Most frequently recommended is Medications and Mother's Milk by Dr. Thomas Hale (noted as "MMM" in the chart above).

Dr. Hale's book provides extensive information on almost every drug out there, including some herbals. For easy reference, he classifies all drugs by safety level (L1 being the safest, L5 being absolutely contraindicated) A woman and her doctor can use Hale to determine whether the drug is safe, what special conditions might be cause for concern, and alternative medication choices. He also includes pharmacological information like a drug's time to its peak plasma level (so if a mother is taking a drug that peaks at 2 hours, she might take it right before her baby's longest sleep stretch of 4-5 hours, to minimize the amount the baby will get). New editions are issued every couple of years and there will be another coming out in 2010.
If a mother or doctor doesn't have access to Hale, a good alternative is LactMed, run by the Toxicology Data Network of the National Library of Medicine.

Like Hale, it includes an overview of published research on the effects of the drug, medication alternatives, and a summary of recommendations. With so many doctors carrying PDAs and/or smartphones that allow them to access online resources, LactMed is an excellent tool to get quick answers. However, unlike Hale, it doesn't assign a safety level or include more detailed pharmacological information.
If your care provider is concerned about breastfeeding and medication use, keep in mind that they may not have the best resources. Investigate further and bring those resources to their attention! If a mom is taking medication that's potentially of concern, the LCs I'm training with will print out a LactMed reference page, or copy the relevant pages in Hale, and tell moms to bring the info to their primary care providers. That way the woman and her care provider can look at the information together and make a decision with all the facts available.
And remember, the question should not be "Is there any risk at all posed by breastfeeding while taking this drug?" - every drug carries theoretical risks, no matter how slight. Instead the question should be "Does the risk of the drug outweigh the risks of NOT breastfeeding?" Most often, the answer is NO!
This is not, of course, all their fault. As La Leche League notes, "Health care givers often turn to the Physicians' Desk Reference (the PDR) for information about drugs. ... Information in the PDR comes directly from pharmaceutical companies, whose first concern is avoiding liability. When there are no studies that prove beyond a doubt that a drug is safe for nursing mothers, the drug companies must advise against using it while breastfeeding - even if what is known about the drug suggests that there is little cause for concern."
What resources your doctor uses to determine the safety of medication can make a big difference. One study used a list of drugs that were commonly prescribed to breastfeeding mothers, and looked how many were considered safe in frequently consulted resources:

From Akus M, Bartick M. Lactation Safety Recommendations and Reliability Compared in 10 Medication Resources Ann Pharmacother. September 2007;41(9):1352-1360.
As you can see, there are much better resources out there than the PDR! Most frequently recommended is Medications and Mother's Milk by Dr. Thomas Hale (noted as "MMM" in the chart above).

Dr. Hale's book provides extensive information on almost every drug out there, including some herbals. For easy reference, he classifies all drugs by safety level (L1 being the safest, L5 being absolutely contraindicated) A woman and her doctor can use Hale to determine whether the drug is safe, what special conditions might be cause for concern, and alternative medication choices. He also includes pharmacological information like a drug's time to its peak plasma level (so if a mother is taking a drug that peaks at 2 hours, she might take it right before her baby's longest sleep stretch of 4-5 hours, to minimize the amount the baby will get). New editions are issued every couple of years and there will be another coming out in 2010.
If a mother or doctor doesn't have access to Hale, a good alternative is LactMed, run by the Toxicology Data Network of the National Library of Medicine.

Like Hale, it includes an overview of published research on the effects of the drug, medication alternatives, and a summary of recommendations. With so many doctors carrying PDAs and/or smartphones that allow them to access online resources, LactMed is an excellent tool to get quick answers. However, unlike Hale, it doesn't assign a safety level or include more detailed pharmacological information.
If your care provider is concerned about breastfeeding and medication use, keep in mind that they may not have the best resources. Investigate further and bring those resources to their attention! If a mom is taking medication that's potentially of concern, the LCs I'm training with will print out a LactMed reference page, or copy the relevant pages in Hale, and tell moms to bring the info to their primary care providers. That way the woman and her care provider can look at the information together and make a decision with all the facts available.
And remember, the question should not be "Is there any risk at all posed by breastfeeding while taking this drug?" - every drug carries theoretical risks, no matter how slight. Instead the question should be "Does the risk of the drug outweigh the risks of NOT breastfeeding?" Most often, the answer is NO!
Monday, February 1, 2010
LC update
I haven't posted about my LC training lately, although the pressure is starting to build on that front! I'm starting to realize how intense this whole "train-in-one-year" thing is. My class is starting a study group to begin preparing for the exam already, realizing that July isn't as far away as we think.
The LCs that we're training with have also begun to turn more responsibility over to us. Last week I did one consult supervised and one almost totally by myself. Both were, of course, simple consults. The first was just fixing a minor latch problem - the mom had suffered through weeks of sore nipples with her first baby, and it was so nice to be able to explain to her that this was not normal, fix the latch, and hear her say "That feels so much better!" The second was mostly just education of a family about how babies are usually not big eaters in the first 24 hours. I also tried to help them get the baby to latch on, because they were so eager to get her eating, but of course she just looked at us like we were crazy. Why were we bothering her? She was busy sleeping! Still, it was good practice.
I am already sensing the need to rein in the ol' talking. I realize it as soon as I leave the room, or even sometimes while I'm still talking: too much information, too many ways to say the same thing, too fast. My goal for this week is to take a deep breath, speak slowly, and pick no more than 2-3 things that I really want to communicate over the course of the day (for example: 1) your baby should wake up to eat soon; 2) keep offering her the breast every 2-3 hours.)
Skills I am getting better at: slipping that little supplementer tube in the corner of the baby's mouth, being confident about identifying and fixing the latch. Skills I am inexplicably getting worse at: setting someone up to use the football hold. What's up with that? As with everything else, I think I'm overthinking it (also, there are never enough pillows at the hospital).
Exciting new project (because I didn't have enough already?): helping a local LC start a new group lactation visit. I am super excited about getting to watch her work/assist her, and about the prospect of helping with this group. I hope we can recruit people to come. She's applied for a grant to do some evaluation of its effectiveness so I'm also helping with some of the logistics for that.
I've been thinking about setting up some other observation visits with other LCs but I'm hesitant to do it in any large-scale way. Every time I start over with a new person, it's a lot of observation so I can learn how they do it and so they can get to trust me. The way I'm feeling right now, I can learn a lot from watching any LC, but I also want to focus my time on practice. You can only observe so much before you just need to start getting hands-on and realize all the other stuff you need to learn. Even after I take the exam, I'd love to shadow LCs I admire, or who have skills that I want to gain. But I also feel like when I take the exam, I should feel like I'm at a place where I am comfortable managing a case from start to finish, and I can't get that by starting over and over with new people.
So that's where it's at right now! I'm almost excited to start studying for the exam. That should tell you how much I love this stuff...
The LCs that we're training with have also begun to turn more responsibility over to us. Last week I did one consult supervised and one almost totally by myself. Both were, of course, simple consults. The first was just fixing a minor latch problem - the mom had suffered through weeks of sore nipples with her first baby, and it was so nice to be able to explain to her that this was not normal, fix the latch, and hear her say "That feels so much better!" The second was mostly just education of a family about how babies are usually not big eaters in the first 24 hours. I also tried to help them get the baby to latch on, because they were so eager to get her eating, but of course she just looked at us like we were crazy. Why were we bothering her? She was busy sleeping! Still, it was good practice.
I am already sensing the need to rein in the ol' talking. I realize it as soon as I leave the room, or even sometimes while I'm still talking: too much information, too many ways to say the same thing, too fast. My goal for this week is to take a deep breath, speak slowly, and pick no more than 2-3 things that I really want to communicate over the course of the day (for example: 1) your baby should wake up to eat soon; 2) keep offering her the breast every 2-3 hours.)
Skills I am getting better at: slipping that little supplementer tube in the corner of the baby's mouth, being confident about identifying and fixing the latch. Skills I am inexplicably getting worse at: setting someone up to use the football hold. What's up with that? As with everything else, I think I'm overthinking it (also, there are never enough pillows at the hospital).
Exciting new project (because I didn't have enough already?): helping a local LC start a new group lactation visit. I am super excited about getting to watch her work/assist her, and about the prospect of helping with this group. I hope we can recruit people to come. She's applied for a grant to do some evaluation of its effectiveness so I'm also helping with some of the logistics for that.
I've been thinking about setting up some other observation visits with other LCs but I'm hesitant to do it in any large-scale way. Every time I start over with a new person, it's a lot of observation so I can learn how they do it and so they can get to trust me. The way I'm feeling right now, I can learn a lot from watching any LC, but I also want to focus my time on practice. You can only observe so much before you just need to start getting hands-on and realize all the other stuff you need to learn. Even after I take the exam, I'd love to shadow LCs I admire, or who have skills that I want to gain. But I also feel like when I take the exam, I should feel like I'm at a place where I am comfortable managing a case from start to finish, and I can't get that by starting over and over with new people.
So that's where it's at right now! I'm almost excited to start studying for the exam. That should tell you how much I love this stuff...